* The preview only shows a few pages of manuals at random. You can get the complete content by filling out the form below.
Description
Relationship between low maternal vitamin D status and the risk of severe preeclampsia: A case control study Authors:SarvinPashapouraSariehGolmohammadloubTaherehBehroozi-LakbcHojjatGhasemnejad-BerenjicdSoniaSadeghpourbMortezaGhasemnejad-Berenjie Source: Retrieved from https://www.sciencedirect.com/science/article/pii/S2210778918306792. Highlights •Pre-eclampsia remains a major cause of maternal death in low-income countries. •Prevalence of Vitamin D Deficiency among Iranian Population is high. •Low maternal concentrations of 25(OH) increase pre-eclampsia risk.
Abstract Background Low maternal vitamin D status has been associated with several adverse outcomes during pregnancy. The aim of the study was to evaluate the vitamin D levels in preeclamptic and healthy pregnant women and the role of vitamin D deficiency in the etiology of preeclampsia. Methods In this case-control study, 80 preeclamptic women and 80 healthy pregnant women were selected from Motahari hospital in Urmia, Iran. 2 ml of venous blood sample was collected from each pregnant woman and the serum 25-OH-D level was measured by Enzyme-Linked Immunosorbent Assay (ELISA) and reported in nanograms per milliliter. levels of 25-OH-D less than 10 ng mL−1, between 10 ng mL−1 and 29 ng mL−1 and more than 30 ng mL−1, were considered as deficient, insufficient and normal 25-OH-D concentrations, respectively. Results were analyzed by independent t-test, Mann-Whitney U test, and logistic regression. Results Preeclamptic women (n = 80) were noted to have decreased total 25-OH-D levels relative to healthy control women (n = 80; P = 0.01). This difference in total 25-OH-D remained significant after control for potential confounders [odds ratio (OR) = 4.79, confidence interval (CI) = 1.45–9.87, P = 0.01]. Conclusion These results showed that vitamin D deficiency has a statistically significant relationship with preeclampsia and support the hypothesis that vitamin D deficiency may be a risk factor for preeclampsia. Keywords PreeclampsiaVitamin DPregnancy25-OH-D 1. Introduction Preeclampsia is a disorder that can happen after 20 weeks of gestation and characterized by high blood pressure (BP ≥ 140/90 mm Hg) and proteinuria. This syndrome occurs in 2–8% of pregnancies and lead to 25% of the perinatal morbidity and mortality all over the world [1]. Factors that may increase the occurrence of preeclampsia include: obesity, diabetes, nulliparity, chronic kidney diseases, chronic hypertension before pregnancy, immune disorders, family history of preeclampsia, twin or multiple pregnancy and a personal history of preeclampsia [2]. The activation of maternal inflammatory system due to abnormal placental development, which induces oxidative stress, is the probable origin of preeclampsia [3]. Recent epidemiological studies have emphasized the role of vitamin D deficiency in the development of preeclampsia [4], [5]. Vitamin D may play a part in the etiology of preeclampsia by modulating immune function and inflammatory response [6] and regulating the transcription and function of genes related to placental normal implantation and angiogenesis [7], [8]. Although many [4], [9], [10], [11], [12] observational studies suggest vitamin D deficiency is a risk factor for preeclampsia, the relation
between maternal vitamin D deficiency and the risk of preeclampsia is still disputed and results of literature review are controversial [13], [14], [15].
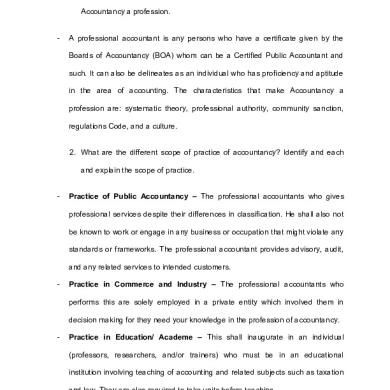
High prevalence of vitamin D deficiency in Iranian women with a special culture and lifestyle [9] and its relation with pregnancy related outcomes and lack of information about the association between vitamin D and preeclampsia in northwest of Iranian women, encouraged us to undertake a study to clarify the link between vitamin D levels and preeclampsia. The aim of this study was to explore the relation between serum vitamin D level and preeclampsia in northwest Iranian women. 2. Material and method 2.1. Study design and population This case–control study was carried out on 80 preeclamptic women, who were selected from Motahari educational hospitals in urmia, northwest of Iran, from January to May 2016. Eighty healthy pregnant women were selected among women who attended motahari hospital with labour pain as the control group (the control group were not matched with the case group). This study was approved by the research and ethics Committee in urmia University of Medical Sciences and written informed consent was obtained from all women recruited into the study. The inclusion criteria were singleton and term pregnancy, no known medical disorders (hypertension, diabetes, kidney, etc.), no history of vitamin D intake during pregnancy, no smoking and no BMI more than 30. The presence of hypertension (systolic blood pressure (SBP) ≥ 140 mmHg and diastolic blood pressure (DBP) ≥ 90 mmHg) on 2 occasions at least 6 h apart after 20 weeks of gestation with detectable proteinuria greater than 0.3 g/24 h was the diagnostic criteria for preeclampsia [16]. A gynecologist confirmed the pre-eclampsia in participants. Details regarding complication in pregnancy, labour and delivery, were collected from the hospital record files and a checklist was utilized for the results of the blood tests. Before labour onset a blood sample (5 ml) was drawn from each participant and sent to the laboratory where the blood samples were centrifuged at 3500 rpm at 4 °C for 10 min and stored at −25 °C until evaluation. 2.2. Laboratory method description The serum 25-OH-D concentration was measured using an Enzyme Linked Immunosorbent Assay (ELISA) and results were reported as ng/ml. The IDS 25-OH-D EIA kit is an enzyme immunoassay for quantitation of 25-OH-D. We classified participants with deficiency if the vitamin D level is <10 ng/ml, between 10 and 30 ng/ml it is considered as insufficiency, and if it is >30 ng/ml, it is considered within the normal range. 2.3. Statistical analyses Data entry and analysis were done using SPSS version 19 (SPSS Inc., Chicago, IL, USA). The Kolmogorov–Smirnov test was used for testing normality. The independent t-test was used for the data with normal distribution. Vitamin level and BMI did not have normal distribution and the Mann–Whitney U test was used for comparing two groups. The chi-square test was used for comparing categorical data between two groups. Logistic regression was used to estimate the effect of vitamin D levels on preeclampsia risk after adjusting for potential confounders (age and BMI). 3. Results In this study, 80 healthy normotensive pregnant women and 80 preeclamptic women were included. Pregnancy demographic and outcomes are summarized in Table 1. Patients with preeclampsia were noted to be older with a greater prepregnancy body mass index. No statistically significant differences were found in gravidity and parity between two groups. Weeks of pregnancy were significantly lower in the preeclamptic group compared to the healthy group (37.6 ± 1.59 and 39.2 ± 1.18 weeks, respectively, p < 0.001). Consequently the two groups showed a significant difference regarding the systolic and diastolic blood pressure (p < 0.001). The mean serum level of 25-OH-D in preeclamptic group was significantly lower than that in the healthy group (15.27 ± 3.52 vs. 23.84 ± 6.93, p < 0.001) as shown in Fig. 1. None of the women in the healthy group demonstrated preeclampsia after delivery. Multiple logistic regressions were used to evaluate the relationship of maternal plasma 25-OH-D on the odds of getting preeclampsia. The adjusted odds ratio showed that Vitamin D deficiency was significantly higher
in the preeclampsia group [odds ratio (OR) = 4.79, confidence interval (CI) = 1.45–9.87, P = 0.01]. Results of this analysis are presented in Table 2. Women with age 30–35 years were more prone to get preeclampsia compared with the healthy group (OR = 2.96, CI = 1.42–4.47, P = 0.01). In this research, women with BMI more than 30 were excluded from study; the results showed that in women with BMI 25 to 29.9, preeclampsia is more common (OR = 3.49, CI = 1.04–5.65, P = 0.01) (Table 2).
Group Preeclampsia (n = 80)
Healthy (n = 80)
women
Variable
Mean ± SD or N (%)
P value
Maternal age (year)
28.83 ± 6.7
24.13 ± 8.4
0.001
BMI (kg m−2)
22.9 ± 5.2
24.3 ± 1.9
0.03
Nulliparous, %
41
39
NS
parity
1.4 ± 1.1
1.2 ± 1.0
NS
Gestational age (week)
37.6 ± 1.59
39.2 ± 1.18
0.001
Systolic blood pressure (mmHg)
151.68 ± 9.3
114.71 ± 5.3
0.001
Diastolic blood pressure (mmHg)
99.42 ± 4.9
71.13 ± 4.8
0.001
Preterm delivery (<37 wks), %
9.25
4.67
0.001
small for gestational ages, %
8.76
5.07
0.001
25-OH-D ng mL−1
15.27 ± 3.52
23.84 ± 6.93
0.001
Deficiency of 25-OH-D% <10 ng mL−1
23
6
0.001
Vitamin D status
Insufficient 25-OH-D% 10–30 ng mL−1 69
74
Normal level of 25-OH-D%
20
8
BMI, body mass index; SD, standard deviation; NS, not significant.
Fig.1. Maternal plasma 25-hydroxyvitamin D in preeclamptic women vs. healthy subjects. Patients with preeclampsia had significantly decreased levels of 25-hydroxyvitamin D relative to healthy control pregnancies that were matched for gestational age at plasma sampling (median 25-hydroxyvitamin D, 15.27 ± 3.52 vs 23.84 ± 6.93 ng/mL; P = 0.001). The probability value was determined by Mann Whitney U test.
Table 2. The unadjusted and adjusted odds ratios for variables related to pre-eclampsia.
Variables
Unadjusted analysis
P-value*
Adjusted analysis
P-value*
Odds ratio (95% CI)†
Odds ratio (95% CI) Deficiency of 25-OH-D
4.68 (1.33–9.57)
0.01
4.79 (1.45–9.87)
0.01
Insufficiency 25-OH-D
0.83 (0.21–2.58)
NS
0.89 (0.18–0.96)
NS
Age 20–30
0.95 (0.71–0.97)
NS
0.97 (0.79–0.99)
NS
Age 30–35
2.48 (1.12–4.29)
0.03
2.96 (1.42–4.47)
0.01
0
1.16 (0.95–1.43)
NS
1.34 (0.93–1.94)
NS
1–2
0.64 (0.36–1.16)
NS
0.71 (0.71–1.84)
NS
≥3
0.84 (0.67, 1.06)
NS
0.91 (0.37, 1.68)
NS
BMI < 20 kg m−2
0.72 (0.17–1.49)
NS
0.81 (0.19–1.56)
NS
BMI 20 to 24.9 kg m−2
1.35 (0.65–2.91)
NS
1.39 (0.83–2.98)
NS
BMI 25 to 29.9 kg m−2
3.14 (1.03–5.26)
0.02
3.49 (1.04–5.65)
0.01
Parity
BMI, body mass index; CI, confidence interval. *BackWald method. Adjusted for age and BMI, NS, not significant. 4. Discussion The present study was aimed to investigate the relationship between preeclampsia which is one of the most serious forms of hypertensive disorders in pregnancy and levels of serum 25-OH-D. Factors that play a role in the pathogenesis of preeclampsia have not yet been completely understood [17]. In recent years various studies have supported the hypothesis of the role of vitamin D in the etiology of preeclampsia [9], [10], [11], [18], [19]. Vitamin D is considered as having an immunomodulatory and anti-inflammatory role in many systems [20], [21], [22] and also has been suggested to play a role in major signal and gene regulations in the early developmental phase of placenta [23] and based on the literatures Placental abnormalities associated with preeclampsia [24]. Furthermore, there is evidence that vitamin D metabolites protect endothelial cells from oxidative stress and minimize the effects of exposure to preeclampsia-related factors [25], [26]. In addition, active vitamin D influences the renin-angiotensinaldosterone system, including the regulation of blood pressure [27]. During pregnancy decidua, placenta and maternal kidney production of 25-OH-D is increased, which in turn can increase the level of vitamin D of mothers. This function is necessary to increase the calcium absorption in the body of the pregnant women in order to increase the calcium requirements of the baby [28]. Various studies have reported that cellular immune abnormalities can negatively affect pregnancy outcome [29]. Vitamin D is thought to play a significant role in modulating of immune responses during pregnancy [8]. It may help mount an appropriate maternal immune response to the placenta preventing the release of anti-angiogenic factors into the bloodstream and modulating hypertension [50]. For example, 1,25(OH)2D suppresses T cell receptor-induced T cell proliferation, altering the cytokine expression profile and diminishing the production of γ-interferon and interleukin-2 [30]. There is a growing interest in the role of maternal vitamin D status in the pathophysiological development of preeclampsia. It has been reported that serum levels of inflammatory cytokines, such as IL-6, TNF- and IL-10, are obviously elevated in women with preeclampsia [31], [32]. Vitamin D has immunosuppressive effects, and vitamin D deficiency is reported to be associated with increased secretion of proinflammatory cytokines in healthy women [33]. In vitro
studies have shown that 1,25(OH)2D3 could modulate IL-6 and TNF-α expression by suppressing NF-κB [34], [35]. It is also found that vitamin D inhibits activation and proliferation of T cells and stimulates the IL-10 secretion and T-regulatory cell production, which are vital in maternal immune tolerance for normal placenta implantation [36].
Acknowledging the role of vitamin D in preeclampsia, this study was done to find out the relationship between preeclampsia and levels of serum 25-OH-D in pregnant women in Iran. A study in Iran showed that 46% of pregnant women during summer and 86% of them during winter had hypovitaminosis D [37]. The social and cultural traditions for the women to cover their skin when going outside their homes and preference of the women to avoid direct sunlight decrease the exposure to sunlight and lead to increase prevalence of vitamin D deficiency in Iranian women [9]. The results of this investigation showed that the mean of 25-OH-D in pre-eclamptic women was significantly lower than in healthy pregnant women. This study finding is consistent with other studies [38], [39]. In 2007 nested case control study by Bodnar et al. showed that Preeclamptic women had 2.5 times more chances of vitamin D deficiency in early pregnancy after adjusting for potential confounders including BMI [4]. Nested case- control study by Baker et al. found that women who had <50 nmol/l (20 ng/ml) of 25-OH-D3 had a 4-fold increase in severe preeclampsia [40]. In 2010, Shin et al. expressed that in pregnancy vitamin D is produced by the placenta and acts on placenta to modulate implantation, cytokine production, and immune response to infection. They concluded that for optimal maternal and neonate health, sufficient vitamin D intake during pregnancy is necessary [41]. In 2011, Dror et al. reported that vitamin D has a key role in regulating the pathways involved in the pathogenesis of preeclampsia [42]. A cohort study in 2009 by Haugen et al. showed that women having higher vitamin D intake (15–20 µg/day as compared to <5 µg/day) had a low rate of preeclampsia (odds ratio [OR] 0.76, 95% CI 0.6–0.95)[43]. Studies in Middle Eastern countries have found that vitamin D deficiency is very common among pregnant women [44], [45]. In 2013 a study by Ullah et al. showed that vitamin D supplementation can effectively lower the risks of both preeclampsia and eclampsia in the pregnant women at risk for vitamin D deficiency [11]. In this study, our results revealed that vitamin D deficiency in pregnancy was associated with almost 5-fold odds of severe preeclampsia (OR = 4.79, CI = 1.45–9.87, P = 0.01). This result is in line with Abedi et al.’s study which reported that vitamin D deficiency is a significant risk (OR = 24.04, CI = 2.10–274.8, P = 0.01) for preeclampsia. Our results showed that there is a statistically significant relationship between 25-OH-D deficiency and preeclampsia. According to these results maternal vitamin D deficiency in pregnancy may be associated with an increased risk of preeclampsia and lower serum concentration of 25-OH-D among preeclamptic women signifies the underlying role of vitamin D deficiency in pathogenesis of the preeclampsia. In this study we did not have the resources to measure serum vitamin D-binding protein (VDBP) in our samples. VDBP increases during pregnancy, whereas 25-OH-D remains constant (38). Our findings, which reflect total (free and bound) 25-OH-D, may therefore overestimate the available 25OH-D to perform physiological functions so we recommend that Future investigations concurrently measure VDBP levels and calculate free vitamin D levels when considering the role of vitamin D in preeclampsia. We also lacked data on PTH concentration, which would have provided a functional indicator of vitamin D status. A limitation of this study was the lack of information on the precise ingestion of vitamin D-containing multivitamins, calcium supplements and long chain fatty acids. Future studies with data on calcium and long chain fatty acids intake and vitamin D status will need to further disentangle the effect of each on preeclampsia risk. Another limitation was the late gestation age at sampling across the two groups. Samples were collected at the time women presented in labor, at one time point. Other studies have shown difference in outcome depending on when the vitamin D sample was collected, i.e. first trimester vs. third trimester. Plausible reason was the late referral of the most pregnant women (after the first trimester) to maternity clinic.
Conflict of interests The authors declare that they have no conflict of interest and that funding was not received for performing the study. Author' contributions
M-ghasemnejad: data collection, analyses and writing the manuscript. S-Pashapour: data collection, project development and approving the manuscript. S-Golmohammadlou: study design, contributed to data collection and manuscript editing. T- Behrouzilak: data collection. H-Ghasemnejad: analyses and approving the manuscript. S-Sadeghpour: analyses and approving the manuscript. Acknowledgements This paper was performed in partial fulfillment of the requirements for a M.D thesis of Sarvin Pashapour at Urmia University of Medical Sciences. We would like to thank the staff of the Motahari educational hospitals for their cooperation during the data collection. References [1]L. Duley The global impact of pre-eclampsia and eclampsia Seminars in Perinatology, Elsevier (2009), pp. 130-137 ArticleDownload PDFView Record in ScopusGoogle Scholar [2]N. Zakiyah, M.J. Postma, P.N. Baker, A.D. van Asselt, I. Consortium Pre-eclampsia diagnosis and treatment options: a review of published economic assessments Pharmacoeconomics, 33 (10) (2015), pp. 1069-1082 CrossRefView Record in ScopusGoogle Scholar [3]S. Saito, A. Shiozaki, A. Nakashima, M. Sakai, Y. Sasaki The role of the immune system in preeclampsia Mol. Aspect Med., 28 (2) (2007), pp. 192-209 ArticleDownload PDFView Record in ScopusGoogle Scholar [4]L.M. Bodnar, J.M. Catov, H.N. Simhan, M.F. Holick, R.W. Powers, J.M. Roberts Maternal vitamin D deficiency increases the risk of preeclampsia J. Clin. Endocrinol. Metab., 92 (9) (2007), pp. 3517-3522 CrossRefView Record in ScopusGoogle Scholar [5]S. Wei, F. Audibert, N. Hidiroglou, K. Sarafin, P. Julien, Y. Wu, Z. Luo, W. Fraser Longitudinal vitamin D status in pregnancy and the risk of pre-eclampsia BJOG: Int. J. Obstet. Gynaecol., 119 (7) (2012), pp. 832-839 CrossRefView Record in ScopusGoogle Scholar [6]M. Hewison Vitamin D and the immune system: new perspectives on an old theme Endocrinol. Metab. Clin. North America, 39 (2) (2010), pp. 365-379 ArticleDownload PDFView Record in ScopusGoogle Scholar [7]S. Chan, R. Susarla, D. Canovas, E. Vasilopoulou, O. Ohizua, C. McCabe, M. Hewison, M. Kilby Vitamin D promotes human extravillous trophoblast invasion in vitro Placenta, 36 (4) (2015), pp. 403-409 ArticleDownload PDFView Record in ScopusGoogle Scholar [8]K.N. Evans, J.N. Bulmer, M.D. Kilby, M. Hewison Vitamin D and placental-decidual function J. Soc. Gynecol. Invest., 11 (5) (2004), pp. 263-271
CrossRefView Record in ScopusGoogle Scholar [9]P. Abedi, Z. Mohaghegh, P. Afshary, M. Latifi The relationship of serum vitamin D with pre-eclampsia in the Iranian women Mater. Child Nutr., 10 (2) (2014), pp. 206-212 CrossRefView Record in ScopusGoogle Scholar [10]E. Hyppönen, A. Cavadino, D. Williams, A. Fraser, A. Vereczkey, W.D. Fraser, F. Bánhidy, D. Lawlor, A.E. Czeizel Vitamin D and pre-eclampsia: original data, systematic review and meta-analysis Ann. Nutr. Metab., 63 (4) (2013), pp. 331-340 CrossRefGoogle Scholar [11]M.I. Ullah, C.A. Koch, S. Tamanna, S. Rouf, L. Shamsuddin Vitamin D deficiency and the risk of preeclampsia and eclampsia in Bangladesh Horm. Metab. Res., 45 (09) (2013), pp. 682-687 View Record in ScopusGoogle Scholar [12]C.L. Wagner, R. McNeil, S.A. Hamilton, J. Winkler, C.R. Cook, G. Warner, B. Bivens, D.J. Davis, P.G. Smith, M. Murphy A randomized trial of vitamin D supplementation in 2 community health center networks in South Carolina Am. J. Obstet. Gynecol., 208 (2) (2013) [13]C.E. Powe, E.W. Seely, S. Rana, I. Bhan, J. Ecker, S.A. Karumanchi, R. Thadhani First trimester vitamin D, vitamin D binding protein, and subsequent preeclampsia Hypertension, 56 (4) (2010), pp. 758-763 View Record in ScopusGoogle Scholar [14]A. Shand, N. Nassar, P. Von Dadelszen, S. Innis, T. Green Maternal vitamin D status in pregnancy and adverse pregnancy outcomes in a group at high risk for pre-eclampsia BJOG: Int. J. Obstet. Gynaecol., 117 (13) (2010), pp. 1593-1598 CrossRefView Record in ScopusGoogle Scholar [15]L.A. Wetta, J.R. Biggio, S. Cliver, A. Abramovici, S. Barnes, A.T. Tita Is midtrimester vitamin D status associated with spontaneous preterm birth and preeclampsia? Am. J. Perinatol., 31 (06) (2014), pp. 541-546 View Record in ScopusGoogle Scholar [16]P. von Dadelszen, L.A. Magee Pre-eclampsia: an update Curr. Hypertens. Rep., 16 (8) (2014), p. 454 Google Scholar [17]J.M. Roberts, C.A. Hubel The two stage model of preeclampsia: variations on the theme Placenta, 30 (2009), pp. 32-37 ArticleDownload PDFView Record in ScopusGoogle Scholar [18]J.L. Faulkner, D.C. Cornelius, L.M. Amaral, A.C. Harmon, M.W. Cunningham, M.M. Darby, T. Ibrahim, S.T. D'Andrea, F. Herse, G. Wallukat
Vitamin D supplementation improves pathophysiology in a rat model of preeclampsia Am. J. Physiol.-Regul. Integr. Comp. Physiol., 310 (4) (2016), pp. R346-R354 CrossRefView Record in ScopusGoogle Scholar [19]J. Tamblyn, R. Susarla, C. Jenkinson, L. Jeffery, O. Ohizua, R. Chun, S. Chan, M. Kilby, M. Hewison Dysregulation of maternal and placental vitamin D metabolism in preeclampsia Placenta, 50 (2017), pp. 70-77 ArticleDownload PDFView Record in ScopusGoogle Scholar [20]T. Caballero-Velázquez, I. Montero, F. Sánchez-Guijo, R. Parody, R. Saldaña, D. Valcarcel, O. López-Godino, C.F. i Coll, M. Cuesta, A. Carrillo-Vico Immunomodulatory effect of vitamin D after allogeneic stem cell transplantation: results of a prospective multicenter clinical trial Clin. Cancer Res., 22 (23) (2016), pp. 5673-5681 CrossRefView Record in ScopusGoogle Scholar [21]A. Hawthorne clinical benefits of vitamin D therapy in inflammatory bowel disease Alimentary Pharmacol. Therap., 45 (10) (2017), pp. 1365-1366 CrossRefView Record in ScopusGoogle Scholar [22] S. Segaert, N.H. Shear, A. Chiricozzi, D. Thaçi, J.-M. Carrascosa, H. Young, V. Descamps Optimizing anti-inflammatory and immunomodulatory effects of corticosteroid and vitamin D analogue fixed-dose combination therapy [23]A. Al-Garawi, V.J. Carey, D. Chhabra, H. Mirzakhani, J. Morrow, J. Lasky-Su, W. Qiu, N. Laranjo, A.A. Litonjua, S.T. Weiss The role of Vitamin D in the transcriptional program of human pregnancy [24]M.L. Falco, J. Sivanathan, A. Laoreti, B. Thilaganathan, A. Khalil Placental histopathology associated with preeclampsia: a systematic review and Meta-Analysis Ultrasound Obstet. Gynecol. (2017) [25]L. Brodowski, J. Burlakov, A.C. Myerski, C.S. von Kaisenberg, M. Grundmann, C.A. Hubel, F. von VersenHöynck Vitamin D prevents endothelial progenitor cell dysfunction induced by sera from women with preeclampsia or conditioned media from hypoxic placenta PloS One, 9 (6) (2014), Article e98527 CrossRefGoogle Scholar [26]F. Uberti, D. Lattuada, V. Morsanuto, U. Nava, G. Bolis, G. Vacca, D. Squarzanti, C. Cisari, C. Molinari Vitamin D protects human endothelial cells from oxidative stress through the autophagic and survival pathways [27]Y.C. Li, J. Kong, M. Wei, Z.-F. Chen, S.Q. Liu, L.-P. Cao 1, 25-Dihydroxyvitamin D 3 is a negative endocrine regulator of the renin-angiotensin system J. Clin. Invest., 110 (2) (2002), pp. 229-238 View Record in ScopusGoogle Scholar [28]F.R. Pérez-López Vitamin D: the secosteroid hormone and human reproduction Gynecol. Endocrinol., 23 (1) (2007), pp. 13-24 CrossRefView Record in ScopusGoogle Scholar
[29]H. Ghasemnejad-Berenji, M.G. Novin, M. Hajshafiha, H. Nazarian, S. Hashemi, B. Ilkhanizadeh, T. Ghasemnejad, S. Sadeghpour, M. Ghasemnejad-Berenji Immunomodulatory effects of hydroxychloroquine on Th1/Th2 balance in women with repeated implantation failure Biomed. Pharmacother., 107 (2018), pp. 1277-1285 ArticleDownload PDFView Record in ScopusGoogle Scholar [30]D.L. Kamen, V. Tangpricha Vitamin D and molecular actions on the immune system: modulation of innate and autoimmunity J. Mol. Med., 88 (5) (2010), pp. 441-450 CrossRefView Record in ScopusGoogle Scholar [31]S.A. McCracken, E. Gallery, J.M. Morris Pregnancy-specific down-regulation of NF-κB expression in T cells in humans is essential for the maintenance of the cytokine profile required for pregnancy success [32]A. Szarka, J. Rigó, L. Lázár, G. Bekő, A. Molvarec Circulating cytokines, chemokines and adhesion molecules in normal pregnancy and preeclampsia determined by multiplex suspension array BMC Immunol., 11 (1) (2010), p. 59 CrossRefGoogle Scholar [33]M.F. Holick Vitamin D deficiency New Engl. J. Med., 357 (3) (2007), pp. 266-281 CrossRefView Record in ScopusGoogle Scholar [34]R.E. Grossmann, S. Zughaier, S. Liu, R. Lyles, V. Tangpricha Impact of vitamin D supplementation on markers of inflammation in adults with cystic fibrosis hospitalized for a pulmonary exacerbation Eur. J. Clin. Nutr., 66 (9) (2012), p. 1072 CrossRefView Record in ScopusGoogle Scholar [35] N. Noyola-Martínez, L. Díaz, E. Avila, A. Halhali, F. Larrea, D. Barrera Calcitriol downregulates TNF-α and IL-6 expression in cultured placental cells from preeclamptic women Cytokine, 61 (1) (2013), pp. 245-250 ArticleDownload PDFView Record in ScopusGoogle Scholar [36] J.S. Adams, M. Hewison Unexpected actions of vitamin D: new perspectives on the regulation of innate and adaptive immunity Nat. Rev. Endocrinol., 4 (2) (2008), p. 80 CrossRefView Record in ScopusGoogle Scholar [37] S.F. Kazemi A, N. Jafari, N. Mousavinasab High prevalence of vitamin D deficiency among women and their newborns in an Iranian population J. Women’s Health, 18 (2009), pp. 835-839 Google Scholar [38] K.M. Baca, H.N. Simhan, R.W. Platt, L.M. Bodnar Low maternal 25-hydroxyvitamin D concentration increases the risk of severe and mild preeclampsia Ann. Epidemiol., 26 (12) (2016), pp. 853-857 e1 View Record in ScopusGoogle Scholar
[39] X. Zhao, R. Fang, R. Yu, D. Chen, J. Zhao, J. Xiao Maternal vitamin D status in the late second trimester and the risk of severe preeclampsia in southeastern China Nutrients, 9 (2) (2017), p. 138 ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar [40] A.M. Baker, S. Haeri, C.A. Camargo Jr, J.A. Espinola, A.M. Stuebe A nested case-control study of midgestation vitamin D deficiency and risk of severe preeclampsia J. Clin. Endocrinol. Metab., 95 (11) (2010), pp. 5105-5109 CrossRefView Record in ScopusGoogle Scholar [41] J.S. Shin, M.Y. Choi, M.S. Longtine, D.M. Nelson Vitamin D effects on pregnancy and the placenta Placenta, 31 (12) (2010), pp. 1027-1034 ArticleDownload PDFView Record in ScopusGoogle Scholar [42]D.K. Dror Vitamin D status during pregnancy: maternal, fetal, and postnatal outcomes Curr. Opin. Obstet. Gynecol., 23 (6) (2011), pp. 422-426 View Record in ScopusGoogle Scholar [43]M. Haugen, A.L. Brantsæter, L. Trogstad, J. Alexander, C. Roth, P. Magnus, H.M. Meltzer Vitamin D supplementation and reduced risk of preeclampsia in nulliparous women Epidemiology (2009), pp. 720-726 View Record in ScopusGoogle Scholar [44]A. Mithal, D.A. Wahl, J.-P. Bonjour, P. Burckhardt, B. Dawson-Hughes, J.A. Eisman, G.E.-H. Fuleihan, R.G. Josse, P. Lips, J. Morales-Torres Global vitamin D status and determinants of hypovitaminosis D Osteopor. Int., 20 (11) (2009), pp. 1807-1820 CrossRefView Record in ScopusGoogle Scholar [45]C. Palacios, L. Gonzalez Is vitamin D deficiency a major global public health problem? J Steroid Biochem. Mol. Biol., 144 (2014), pp. 138-145 © 2019 International Society for the Study of Hypertension in Pregnancy. Published by Elsevier B.V. All rights reserved.