* The preview only shows a few pages of manuals at random. You can get the complete content by filling out the form below.
Description
J Istanb Univ Fac Dent. 2016; 50(1): 51–54. Published online 2016 Jan 12. doi: 10.17096/jiufd.77437 PMCID: PMC5573453 PMID: 28955555
Tooth extraction from a patient with cavernous hemangioma in maxillofacial region: case report Onur Dincer Kose,1,* Cem Tanyel,1 Taha Emre Kose,2 Mehmet Ali Erdem,1 and Abdulkadir Burak Cankaya1 Author information Article notes Copyright and License information Disclaimer
Abstract Go to:
Introduction The term hemangioma is a common term which is used to describe many vascular anomalies but essentially states benign humoral lesions that shows rapid growth period with endothelial cell proliferation and following involution phase. Generally, they are not present at birth and become evident in the first 8 weeks of life (1). Hemangiomas are mostly asymptomatic and they are usually located in cutaneous and mucosal areas. They are rarely seen at jaws. If there is no complication related to the tumor, treatment is not necessary for these lesions. The purpose of this report is to describe the surgical management of a patient with hemangioma located in her right cheek. Go to:
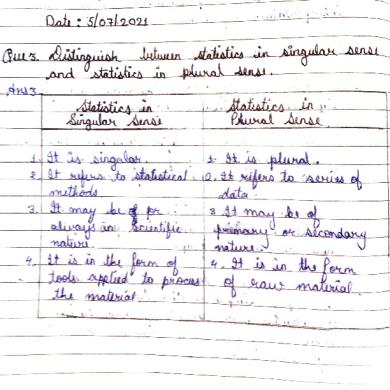
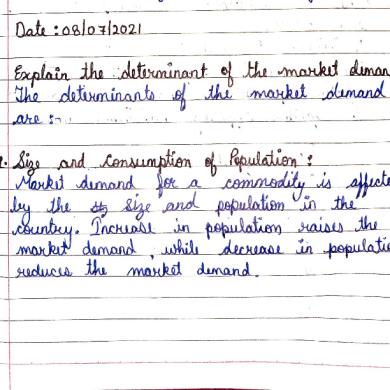
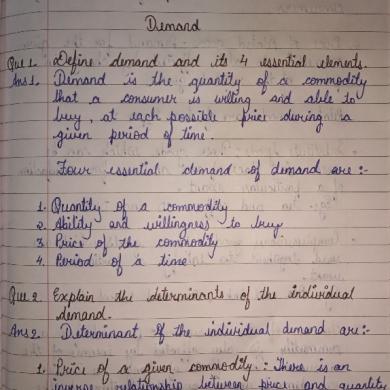
Case Report A 39 year-old female patient has been referred to our clinic for dental complaints. Patient’s medical history revealed mild asthma and hemangioma located at her right cheek which was diagnosed in childhood (Figure 1). Clinical examination revealed swelling, blue-purple discoloration at her right cheek and vestibular sulcus (Figure 2). Patient’s condition was consulted with Interventional Radiology Clinic. Because lesion was located deeply no treatment was planned and routine follow-up was suggested due to tissue necrosis risk after embolization or sclerotherapy. It was reported that venous distension due to the lesion’s hyper vascularity may cause hemorrhage complication after oral surgery. Clinical and radiologic examination revealed advanced periodontal bone loss around teeth no: 12 and 13 (FDI Classification) and hypermobility (Figure 3). Based on these, extraction of 12-13 was planned. Contrast-enhanced MRI showed a lesion with multiple compartments and its size was measured as 4.5 X 5.5 cm. Lesion was located in the right facial fatty tissues and near premaxillary area. Lesion demonstrated hyper intensity at T2A sequences and also in peripheral contrast enhancement on MRI. Therefore, it was concluded that the lesion did not reach the alveolar crest (Figure 4). Teeth numbered 12 and 13 were extracted following local anesthesia, gelatin sponges (SPONGOSTAN, Ferrosan, Denmark) were placed in the sockets
and the wound was sutured (Figure 5). Hemostasis was obtained and sutures were removed at postoperative 7th day. Healing was uneventful.
Figure 1. Asymmetry and discoloration at patient’s right cheek.
Figure 2. Intraoral appearence of cavernous hemangioma.
Figure 3. Panoramic radiography of the patient.
Figure 4. MRI image of the lesion (axial slice, green arrows indicate the area affected by the lesion).
Figure 5. Postoperative intraoral appearence.
Go to:
Discussion Hemangiomas are benign tumors mostly located in soft tissues. They are categorized into 2 subtypes as capillary and cavernous depending on size of the area filled with blood. Also, a third type called juvenile hemangioma also reported (2). Capillary hemangiomas are characterized with capillary structure with proliferative activity. They arise and regress in a short time (3). Most of the hemangiomas are cavernous type. Initially, cavernous hemangiomas were thought to be congenital but, recently, the autosomal dominant genetic pattern is suggested. Cavernous hemangiomas are characterized by mitotic activity, large vascular structures and long clinical history (4). In our case, long clinical history was present. MRI findings revealed the lesion as a cavernous type hemangioma. Hemangiomas are the most frequent tumors of first decade which are mostly located in cutanous and mucosal regions (5). Central types of the hemangiomas are often seen in vertebrae and skull. They are rarely seen in jaws and mandible/maxilla ratio is 2:1. The most common locations for mandibular hemangiomas are posterior area, ramus and inferior alveolar canal (6). Female/male ratio is 3-5:1 and they are diagnosed in Caucasians more frequently (7). Every 1 of 4 newborns who are under weight of 1000 g have been reported to have hemangiomas (1, 8). Although hemangiomas are relevant to the organ in which they are located, they do not include its parenchyma (5). Early period of hemangiomas presents abundant endothelium cells and indistinct vascular lumen. As the lesion maturates, the endothelium cells become straight and capillary spaces become clear. By the involution of the hemangioma, vascular spaces become less clear and fibrosis occurs. Differential diagnosis for hemangiomas must be done with vascular anomalies which are structural. Vascular anomalies are present at birth and they do not regress (7). Hemangiomas are usually asymptomatic besides cosmetic concerns. Fully developed hemangiomas are rare at birth (7). They show a rapid growth phase at first weeks and this phase takes nearly 6-7 months (7, 9). Superficial hemangiomas in this stage are pulsatile,
warm, tense, swallowed and shiny red colored lesions. They represent high flow and murmur in physical examination (9). Deep tumors clinically shows only a bluish discoloration in the relevant area (7). Proliferative phase takes 6 to 10 months and after that regression period begins. This period continues until the patient is nearly two years old. In this period, tumour growth starts to slowing down and involution begins. Lesions change its color to purple and become softer in palpation. The regression period takes 5 to 7 years. 50% of all hemangiomas completely involute by the age of 5 years, and, 90% by the age of 9 years. In half of the patients, after tumor regression normal skin appearance can be observed. However, in 40% of the patients, atrophy, scar, wrinkles and telangiectasia are seen. On the other hand, glucose transporter 1(GLUT1) which is a immunohistochemical marker is positive in infants who have hemangiomas. In other vascular malformations, GLUT1 was reported to be negative (7). For hemangioma detection, diagnostic methods are computerized tomography(CT), MRI, ultrasonography and arteriography (3). In panoramic radiography, they may show well or illdefined borders. This depends on the amount of residual bone around hemangioma (6). Central hemangioma demonstrates as soap bubble appearance or as honeycomb shaped osteolytic defects in panoramic radiography (10). In CT, they show as homogeneous osteolytic areas with sharp borders. Their attenuation values are lower than the muscles. In contrast enhancement they show a gradual enhancement (11). At MRI, T1 weighted images show moderate and T2 weighted images show strong signal increase (3). They show moderate or high echogenicity at ultrasound images. At Doppler scans, they may show low blood flow (12). Calcifications may be seen in sclerozed hemangiomas (13). In our case, MRI images showed a lesion with multiple compartments and hyper intensity in T2A, which is located in right facial fatty tissues in the premaxillary area. Lesion also presented contrast enhancement at MRI, however, there was no sign in the panoramic radiography. Complications may arise in 40% of hemangiomas. The most frequent problem is ulceration. Hemorrhage is not serious and compression is often enough for hemostasis. Secondary infection may cause serious conditions like osteomyelitis, especially in deeply penetrated lesions. Periocular hemangiomas cause amblyopia, strabismus or astigmatism whereas hemangiomas in airway cause nutritional and inspiratory problems. Hemangiomas in the otic region cause otitis and hearing loss. Multiple cutaneous or large facial hemangiomas must be further investigated to determine their relation to visceral hemangiomas (7, 9). Treatment is indicated when symptoms like pain, infection, ulceration, airway obstruction, cosmetic deformation and hemorrhage in which hemostasis could not be obtained are present. Systemic or intra lesional steroids, injection of sclerozing agents, radiotherapy, cryotherapy, vascular ligation, embolization and surgical excision are treatment options for hemangiomas. Selection of treatment method depends on the lesion’s characteristics (3). Corticosteroids are the first step of medical therapy. Daily doses of 2-4 mg/kg taken orally are prescribed (4). Intra lesional and topical corticosteroids are indicated in problematic, localized and small lesions (7). For aggressive and steroid insensitive lesions, the interferon alpha and vincristine therapy are indicated. Propranolol induces vasoconstriction by beta-adrenergic effect and this leads to discoloration and softening of lesion in first 24 hours. Propranolol also reduces the growth factor levels and increases the cellular apoptosis (14). Whenever the medical therapy fails, surgical methods such as sclerozing agent injection, cryosurgery and carbon dioxide laser therapy are indicated (4). In our case, sclerotherapy and embolization were planned because of deep location of the lesion, however, in the presence of necrosis risk; routine follow up decision was made. Go to:
Conclusion Although being treatable, the hemangioma still represents a complex entity which should be classified more efficiently. This lesion should be always considered in the differential diagnosis of soft tissue lesions. Planning of the oral surgery procedures should focus on the determination of the lesion’s relation with neighboring anatomical structures based on careful clinical and radiological examination in order to avoid life-threatening complications. Go to:
Footnotes Source of funding: None declared. Conflict of interest: None declared.
Go to:
References 1. Sevinir B. Çocukluk çağında hemanjiomlar Pediatri 2006;4(2):63–68. [Google Scholar]
ve
klinik
özellikleri. Güncel
2. Waal IS. Benign tumors and tumor-like lesions. Hamilton: B C Decker Inc; 1998. pp. 1407–17. [Google Scholar] 3. Kiymaz N, Yilmaz N, Ozen S, Demir I, Gudu BO, Kozan A. Cavernous hemangioma presenting as a giant cervical mass: a case report. Turk Neurosurg 2010. January;20(1):69– 72. [PubMed] [Google Scholar] 4. Joseph S, Prakash M, Mohammed HK, Govar A. Benign mass in tonsil- cavernous hemangioma. J Clin Diagn Res 2013. October;7(10):2284–2285. [PMC free article] [PubMed] [Google Scholar] 5. Doğan RK, Eren SB. Intramasseter hemanjiom. Türk Otolarengoloji Arşivi 2012;50(3):46– 49. 10.5152/tao.2012.14 [CrossRef] [Google Scholar] 6. Goaz PW. Oral radiology principles & interpretation. St. Louis (Missouri): Mosby Elsevier; 1994. [Google Scholar] 7. Neville BW, Allen CM, Bouquot JE. Oral and maxillofacial pathology. St. Louis (Missouri): Saunders Elsevier; 2009. pp. 538–43. [Google Scholar] 8. Smolinski KN, Yan AC. Hemangiomas of infancy: clinical and biological characteristics. Clin Pediatr (Phila) 2005. Nov-Dec;44(9):747–766. 10.1177/000992280504400902 [PubMed] [CrossRef] [Google Scholar] 9. Işık MD, Görmüş N. Hemanjiomlarda cerrahi tedavi. Damar Cer Derg 2012;21(2):81– 86. [Google Scholar] 10. Dhupar V, Yadav S, Dhupar A, Akkara F. Cavernous hemangioma—uncommon presentation in zygomatic bone. J Craniofac Surg 2012. March;23(2):607–609. 10.1097/SCS.0b013e31824cd7c4 [PubMed] [CrossRef] [Google Scholar] 11. Som PM. Head and neck imaging. St. Louis: Mosby; 2003. [Google Scholar]
12. Ko F, DiBernardo CW, Oak J, Miller NR, Subramanian PS. Confirmation of and differentiation among primary vascular lesions using ultrasonography. Ophthal Plast Reconstr Surg 2011. Nov-Dec;27(6):431–435. 10.1097/IOP.0b013e31822323af [PubMed] [CrossRef] [Google Scholar] 13. Aspestrand F, Kolbenstvedt A. Vascular mass lesions and hypervascular tumors in the head and neck. Characteristics at CT, MR imaging and angiography. Acta Radiol 1995. March;36(2):136–141. [PubMed] [Google Scholar] 14. Zimmermann AP, Wiegand S, Werner JA, Eivazi B. Propranolol therapy for infantile haemangiomas: review of the literature. Int J Pediatr Otorhinolaryngol 2010. April;74(4):338–342. 10.1016/j.ijporl.2010.01.001 [PubMed] [CrossRef] [Google Scholar]