* The preview only shows a few pages of manuals at random. You can get the complete content by filling out the form below.
Description
MHAM-COLLEGE OF MEDICINE DEPARTMENT OF ANATOMY SECTION OF HISTOLOGY
Name:_GONZALEZ, JAMAICA CARYL N. ___Yr.&sec.___1A_____Date:____10/28/2021_
Exercise #12 RESPIRATORY SYSTEM A. Specimen: TRACHEA BRONCHUS (EXTRAPULMONARY) Laboratory Instructions: Focus on the trachea and bronchus. Identify the layers and the components of each layer. Draw and label accordingly. Layers: Mucosa Lining epithelium Lamina Propia Submucosa Seromucous tracheal glands Adventitia Hyaline Cartilage Trachealla or bronchial muscle
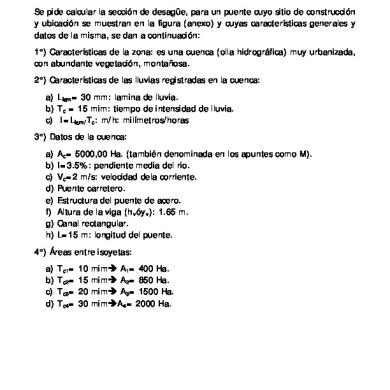
Questions: 1. What are the components of the conducting portion of the respiratory tract? Consists of the nasal cavities, pharynx, larynx, trachea, bronchi (Gr. bronchos, windpipe), bronchioles, and terminal bronchioles 2. Differentiate the extrapulmonary from the intrapulmonary bronchi. Extrapulmonary air conduits are located outside of the lungs and begin with the nose, pharynx and larynx. The trachea is continuous with the larynx above and the two primary bronchi below. It is the supporting framework for 16-20 Cshaped hyaline cartilages. These cartilage "bracelets" are open on the posterior wall of the trachea adjacent to the esophagus. A bundle of smooth muscle fibers bridges the gap between the two ends of the cartilage. Intrapulmonary air conduits extend from the intralobar bronchi to the terminal bronchioles. When the bronchi enter the lung, the C-shaped cartilages that characterize the trachea and primary bronchi are replaced by irregular plates or cartilage that completely surround the cylindrical muscular airway tube. Cartilage disappears in the terminal bronchioles, which have narrowed to a diameter of 1 millimeter. The terminal bronchioles initially have a ciliated columnar epithelium that soon transitions to a low cuboidal epithelium. Mucous and seromucous glands and diffuse lymphatic tissue are associated with smaller bronchi but are not found distal to the region where there is a loss of cartilage plates.
B. Specimen: LUNGS Laboratory Instructions: Study the lungs and identify the different segments of the respiratory tract seen. Note the lining epithelium, presence of glands, goblet cells and cartilage.
a. Intrapulmonary bronchi b. Terminal bronchiole c. Respiratory bronchiole d. Alveolar duct e. Atria f. Alveolar sac g. Alveoli h. Interalveolar septum
Questions: 1. What are the components of the respiratory portion of the respiratory system? Where the system’s main function of gas exchange occurs, consisting of respiratory bronchioles, alveolar ducts, and alveoli. 2. What composes the blood-air barrier? The barrier between capillary blood and alveolar air comprising the alveolar epithelium and capillary endothelium with their adherent basement membranes and epithelial cell cytoplasm. Gaseous exchange occurs across this membrane.
RESPIRATORY SYSTEM Learning Objectives Given written problems and microscopic slides, the students should be able to: 1. Identify the components of the conducting and respiratory portion of the respiratory system and describe their functions. PORTION
CONDUCTING PORTION
COMPONENTS Nasal Cavity
FUNCTIONS Humidify and warm the inspired air. Removes minute airborne particles and other debris before the air reaches the lower airways.
Larynx
Passage for air between the pharynx and the trachea. To maintaining an open airway, movements of these cartilages by skeletal muscles participate in sound production during phonation
Pharynx
It serves both the respiratory and digestive systems by receiving air from the nasal cavity and air, food, and water from the oral cavity.
Trachea
Conduct air to primary bronchi entering lungs; some MALT
Bronchi
Repeated branching; conduct air deeper into lungs
RESPIRATORY PORTION
Bronchioles
Conduct air; important in bronchoconstriction and bronchodilation
Terminal Bronchioles
Conduct air to respiratory portions of lungs; exocrine club cells with several protective and surfactant functions
Respiratory Bronchioles
Conduct air deeper, with some gas exchange, and protective and surfactant functions of club cells
Alveolar Ducts
Conduct air, with much gas exchange
Alveoli
Sites of all gas exchange; surfactant from type II pneumocytes; dust cells
2. Understand how its component parts enhances its functional distribution to the whole system. The respiratory system consists of two components, the conducting portion, and the respiratory portion. The conducting portion brings the air from outside to the site of the respiration. The respiratory portion helps in the exchange of gases and oxygenation of the blood. 3. Enumerate the three divisions of the respiratory system and the components of each. DIVISIONS COMPONENTS THE AIRWAY
Mouth, nose,sinuses, pharynx, trachea, larynx, and bronchial tubes,
THE LUNGS
Alveoli, bronchioles, Capillaries, lung lobe, and pleura
THE MUSCLES OF RESPIRATION
Diaphragm and ribs
4. Compare the right and left lung. CRITERIA Location
Structure
LEFT LUNG It is located on the left side of the respiratory system The diaphragm separates the base of the lung from the stomach and the spleen It is narrow and long
Bronchus
There is only one bronchus
Lobes
It has two lobes, a superior lobe, and an inferior lobe
Number of bronchopulmonary segments
The lobes are further divided into the bronchopulmonary segments. The left lung has 9-10 segments. The left lung is lighter than the right lung. The approx weight of the left lung is 650 gm The left lung shares space with the heart It has one fissure. This fissure is oblique.
Diaphragm
Weight
Shares space with Number of fissures
RIGHT LUNG It is located on the right side The diaphragm separates the base of the lung from the liver It is wider and 5 cms shorter than the left lung. There are two bronchi in the right lung There are three lobes in the right lung; superior lobe, middle lobe, and inferior lobe It has 10 segments.
The right lung is heavier. The approx weight of the right lung is 700 gm The right lung shares its space with the liver It has two fissures, one oblique and one horizontal. The oblique fissure separates the inferior lobe from the middle and superior lobes. The horizontal fissure separates the superior from the middle lobe
5. Describe the respiratory tract walls in terms of the arrangement, composition, and function of their layers and cells. There are four main histological layers within the respiratory system: respiratory mucosa, which includes epithelium and supporting lamina propria, submucosa, cartilage and/or muscular layer and adventitia. Respiratory epithelium is ciliated pseudostratified columnar epithelium found lining most of the respiratory tract; it is not present in the larynx or pharynx. The epithelium classifies as pseudostratified; though it is a single layer of cells along the basement membrane, the alignment of the nuclei is not in the same plane and appears as multiple layers. The role of this unique type of epithelium is to function as a barrier to pathogens and foreign particles; however, it also operates by preventing infection and tissue injury via the use of the mucociliary elevator. Function: Just as the skin protects humans from external pathogens and irritants, the respiratory epithelium acts to protect and effectively clear the airways and lungs of inhaled pathogens and irritants. The division of the respiratory system into conducting and respiratory airways delineates their function and roles. The conducting portion, consisting of the nose, pharynx, larynx, trachea, bronchi, and bronchioles, which all serve to humidify, warm, filter
air. The respiratory portion is involved in gas exchange. There are three major types of cells found in respiratory epithelium, and each holds a vital role in regulating how humans breathe. If any of these components of the barrier are not properly functioning, the body becomes susceptible to acquiring infections, pathogens or inducing inflammation, and disturbing hemostasis. • Humidification & Warming • Filtration • Oxidant defense & Response to Injury • Gas Exchange
6. Distinguish between respiratory tract components based on the difference in the wall structure. • The Nose and its Adjacent Structures- the external nose consists of the surface and skeletal structures that result in the outward appearance of the nose and contribute to its numerous functions. Underneath the thin skin of the nose are its skeletal features. While the root and bridge of the nose consist of bone, the protruding portion of the nose is composed of cartilage. • Pharynx- The pharynx is a tube formed by skeletal muscle and lined by mucous membrane that is continuous with that of the nasal cavities. The pharynx is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx. • Larynx- The larynx is a cartilaginous structure inferior to the laryngopharynx that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs. • Trachea- The trachea (windpipe) extends from the larynx toward the lungs. The trachea is formed by 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are connected by dense connective tissue. The trachealis muscle and elastic connective tissue together form the fibroelastic membrane, a flexible membrane that closes the posterior surface of the trachea, connecting the C-shaped cartilages. The fibroelastic membrane allows the trachea to stretch and expand slightly during inhalation and exhalation, whereas the rings of cartilage provide structural support and prevent the trachea from collapsing. • Bronchial Tree- The trachea branches into the right and left primary bronchi at the carina. These bronchi are also lined by pseudostratified ciliated columnar epithelium containing mucusproducing goblet cells. The carina is a raised structure that contains specialized nervous tissue that induces violent coughing if a foreign body, such as food, is present. Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent their collapse. • Alveoli an alveolar duct - is a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts.
7. Describe the structure of the interalveolar Septum.
Between neighboring alveoli lie thin interalveolar septa consisting of scattered fibroblasts and sparse extracellular matrix (ECM), notably elastic and reticular fibers, of connective tissue. The arrangement of elastic fibers enables alveoli to expand with inspiration and contract passively with expiration; reticular fibers prevent both collapse and excessive distention of alveoli. The interalveolar septa are vascularized with the richest capillary networks in the body
8. Identify the histologic components of the blood-air barrier and describe the function of the blood-air barrier. The densely anastomosing pulmonary capillaries within the interalveolar septa are supported by the meshwork of reticular and elastic fibers in the alveolar walls. Air in the alveoli is separated from capillary blood by three components referred to collectively as the respiratory membrane or blood-air barrier: • Two or three highly attenuated, thin cells lining the alveolus • The fused basal laminae of these cells and the endothelial cells of capillaries • The thin capillary endothelial cells
9. Compare sympathetic and parasympathetic effects on bronchial smooth muscle. The muscle is relaxed and increase the bronchiole diameter by stimulating the sympathetic nervous system while the bronchial spasm is due to the activation of parasympathetic nervous system because it can cause bronchoconstriction to the bronchial muscle.
10. Describe the structure, function, and location of the pleura. The lung’s outer surface and the internal wall of the thoracic cavity are covered by a serous membrane called the pleura. The membrane attached to lung tissue is called the visceral pleura and the membrane lining the thoracic walls is the parietal pleura. The two layers are continuous at the hilum and are both composed of simple squamous mesothelial cells on a thin connective tissue layer containing collagen and elastic fibers. The elastic fibers of the visceral pleura are continuous with those of the pulmonary parenchyma. Between the parietal and visceral layers, the narrow pleural cavity is entirely lined with the mesothelial cells producing a thin film of serous fluid, which acts as a lubricant, facilitating the smooth sliding of one surface over the other during respiratory movements.
11. Identify the organ, tissues and cell types present and distinguish among the various components of the respiratory system microscopically of respiratory tract or lung tissue. RESPIRATORY
LUNGS
12. Identify the layers of the wall of some parts of the respiratory system particularly the trachea and bronchi. The wall of the trachea can be divided into four layers: • mucosa, • submucosa, • musculocartilaginous layer, and
• adventitia.
13. Identify the cells comprising the respiratory system, particularly the cells in the lung parenchyma. The lung parenchyma comprises a large number of thin-walled alveoli, forming an enormous surface area, which serves to maintain proper gas exchange. The alveoli are held open by the Trans-pulmonary pressure, or pre-stress, which is balanced by tissues forces and alveolar surface film forces. Gas exchange efficiency is thus inextricably linked to three including local ventilation, regional blood flow, tissue stiffness, smooth muscle contractility, and alveolar stability. The main pathway for stress transmission is through the extracellular matrix. Thus, the mechanical properties of the matrix play a key role both in lung function and biology. These mechanical properties in turn are determined by the constituents of the tissue, including elastin, collagen, and proteoglycans. In addition, the macroscopic mechanical properties are also influenced by the surface tension and, to some extent, the contractile state of the adherent cells.
14. Identify some diseases that have histologic/pathologic relations with matters discussed above. Pneumonia: An infection of your alveoli, usually by bacteria or viruses, including the coronavirus that causes COVID-19. Tuberculosis: Pneumonia that slowly gets worse, caused by the bacteria Mycobacterium tuberculosis. Emphysema: This happens when the fragile links between alveoli are damaged. Smoking is the usual cause. (Emphysema also limits airflow, affecting your airways.) Pulmonary edema: Fluid leaks out of the small blood vessels of your lung into the air sacs and the area around them. One form is caused by heart failure and back pressure in your lungs’ blood vessels. In another form, injury to your lung causes the leak of fluid. Lung cancer: It has many forms and may start in any part of your lungs. It most often happens in the main part of your lung, in or near the air sacs. Acute respiratory distress syndrome (ARDS): This is a severe, sudden injury to the lungs from a serious illness. COVID-19 is one example. Many people who have ARDS need help breathing from a machine called a ventilator until their lungs recover. Pneumoconiosis: This is a category of conditions caused by inhaling something that injures your lungs. Examples include black lung disease from coal dust and asbestosis from asbestos dust