* The preview only shows a few pages of manuals at random. You can get the complete content by filling out the form below.
Description
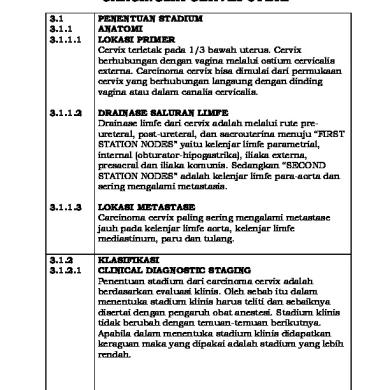
FIGO (International Federation of Gynecology and Obstetrics) Staging System for Carcinoma of the Cervix I - The carcinoma is strictly confined to the cervix (extension to the corpus would be disregarded). I. A - Invasive carcinoma, which can be diagnosed by microscopy, with deepest invasion less than equal to (≤) 5 mm and largest extension less than equal to (≤) 7 mm. I. A1 Measured stromal invasion of less than equal to (s) 3 mm in depth and extension of less than equal to(≤) 7 mm. I. A2 Measured stromal invasion of more than (>) 3 mm and not more than 5 mm in depth with an extension of not greater than >) 7 mm. I. B Clinically visible lesions limited to the cervix uteri or pre-clinical cancers greater than stage IA. All gross lesions, even with superficial invasion, are stage I B cancers. I. B1 Clinically, visible lesion less than equal to (≤) 4 cm in greatest dimension. I. B2 Clinically, visible lesion greater than (>) 4 cm in greatest dimension. I. II. A II. A1 II. A2 II. B II. III. A III. B
Cervical carcinoma extends beyond the uterus but not to the pelvic wall or to the lower third of vagina. Without parametrical invasion. Clinically visible lesion less than equal (s) 4.0 cm in greatest dimension Clinically visible lesion greater than (>) 4.0 cm in greatest dimension. With obvious parametrial invasion. The tumor extends to the pelvic wall and/or involves the lower one third of the vagina and/or causes hydronephrosis or nonfunctioning kidney. Tumor involves lower third of vagina, with no extension to the pelvic wall. Extension to the pelvic wall and/or hydronephrosis or non-
functioning kidney. III. IV. A IV. B
The carcinoma has extended beyond the true pelvis or has involved (biopsy proven) the mucosa of the bladder or rectum. Spread of the growth to adjacent organs. Spread to distant organs.
Management by stages of the disease: Stage IA: Stage IA, without lymph vascular invasion. The This is managed by conservative surgery, i.e. i. ii.
Excisional conization (In case preservation of fertility is desired) Extrafascial hysterectomy Patients treated with conization should be followed closely with: Pap smear Colposcopy > Every 3 months for the first year. ECG For medically by inoperable patients, stage IA carcinoma can be effectively treated with chemoradiation.
Stage IA2: This stage is associated with positive pelvic lymph node in 5% of cases. The preferred treatment of these lesions is modified radical (Class II) hysterectomy with pelvic lymphadenectomy. In patients who desire preservation of fertility, radical trachelectomy with laproscopic or extraperitoncal lymphadenectomy may be performed. In radical trachelectomy cervical and vaginal branches of the uterine artery are ligated, while the main trunk of the uterine artery is preserved. Once the blood supply has been controlled, the cervix is amputated at a point approximately 5 mm caudal to the uterine isthmus. Stage 1B, 112, 11 A: Here, radical hysterectomy (Class III hysterectomy) and radiation are equally effective in treating stages 13 and 11 carcinomas of the cervix. Management of patients with bulky stage I disease (IB) is controversial. The two options are class III hysterectomy or radiation. Often surgery is first performed with postoperative radiation Alternatively, a gynecological oncology group study showed that
weekly cisplatin 40 mg/m' six doses with external radiation and a single implant to give 55 Gy at point R, followed by extrafascial hysterectomy gave the best results. Stages II B, III, IV A, IV B: i. ii. iii. iv.
For stage II B: Radiation therapy is the treatment of choice or radiotherapy followed by radical surgery or radical surgery followed by radiotherapy. For stage III: Here, radiotherapy with routine use of chemotherapy is expected to produce a good prognosis. For IV A: In this stage, palliative radiotherapy, ultra-radical surgery, chemotherapy are the choices of treatment. Stage IV B: These patients have uniformly poor prognosis regardless of treatment, modality.So, chemotherapy is used.
FIGO (International Federation of Gynecology and Obstetrics) Staging System for Carcinoma of the Cervix STAGE I.
I. A
I. A1
I. A2
I. B
I. B1 I. B2
DESCRIPTION The carcinoma is strictly confined to the cervix (extension to the corpus would be disregarded). Invasive carcinoma, which can be diagnosed by microscopy, with deepest invasion less than equal to (≤) 5 mm and largest extension less than equal to (≤) 7 mm. Measured stromal invasion of less than equal to (s) 3 mm in depth and extension of less than equal to(≤) 7 mm. Measured stromal invasion of more than (>) 3 mm and not more than 5 mm in depth with an extension of not greater than >) 7 mm. Clinically visible lesions limited to the cervix uteri or pre-clinical cancers greater than stage IA. All gross lesions, even with superficial invasion, are stage I B cancers. Clinically, visible lesion less than equal to (≤) 4 cm in greatest dimension. Clinically, visible lesion
greater than (>) 4 cm in greatest dimension. II.
II. A II. A1
II. A2 II. B
III.
III. A III. B
IV.
IV. A IV. B
Cervical carcinoma extends beyond the uterus but not to the pelvic wall or to the lower third of vagina. Without parametrical invasion. Clinically visible lesion less than equal (s) 4.0 cm in greatest dimension Clinically visible lesion greater than (>) 4.0 cm in greatest dimension. With obvious parametrial invasion. The tumor extends to the pelvic wall and/or involves the lower one third of the vagina and/or causes hydronephrosis or nonfunctioning kidney. Tumor involves lower third of vagina, with no extension to the pelvic wall. Extension to the pelvic wall and/or hydronephrosis or nonfunctioning kidney. The carcinoma has extended beyond the true pelvis or has involved (biopsy proven) the mucosa of the bladder or rectum. Spread of the growth to adjacent organs. Spread to distant organs.